ISCHEMIC STROKE
Wake-up stroke (WUS)
Updated on 15/10/2024, published on 15/10/2024
Definition
- a Wake-Up Stroke (WUS) refers to a scenario in which a patient wakes up with stroke symptoms, making it difficult to determine the exact time of onset
- this situation is particularly relevant in the management of ischemic stroke, as treatment options depend on the time elapsed since the symptom onset
- original criteria excluded this quite large group of patients from thrombolysis, but this has changed in recent years
- growing evidence suggests that many wake-up strokes occur close to awakening and that patients may still be within the approved time window
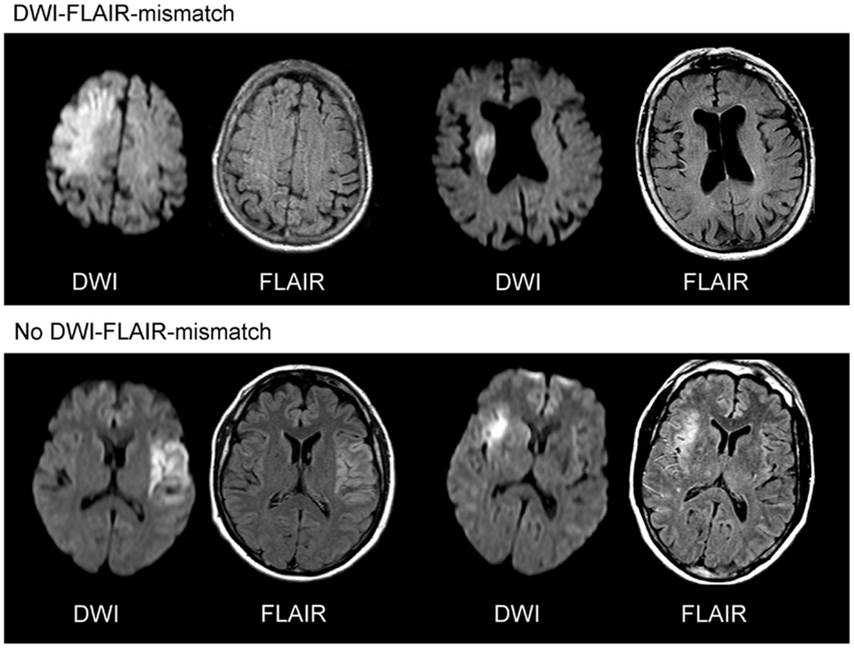
- several imaging techniques show similar findings in WUS patients and those with stroke within 3 or 4.5 h (mismatch on CTP, DWI/FLAIR mismatch, similar early ischemic changes burden, etc.)
- imaging techniques used with the concept of the midpoint of sleep improve thrombolysis availability in WUS patients
Trials
- a meta-analysis of the WAKE-UP, EXTEND, THAWS, and ECASS-4 trials found that thrombolysis indicated by advanced imaging is safe and effective [Thomalla, 2020]
- IV alteplase resulted in a better functional outcome at 90 days than placebo or standard therapy
- a net benefit was observed for all functional outcomes despite an increased risk of sICH
- although there were more deaths with alteplase than with placebo, there were fewer cases of severe disability or death
- if the patient is a candidate for both IVT and MT, IVT is more likely to be performed before MT (expert consensus) (ESO guidelines 2021)
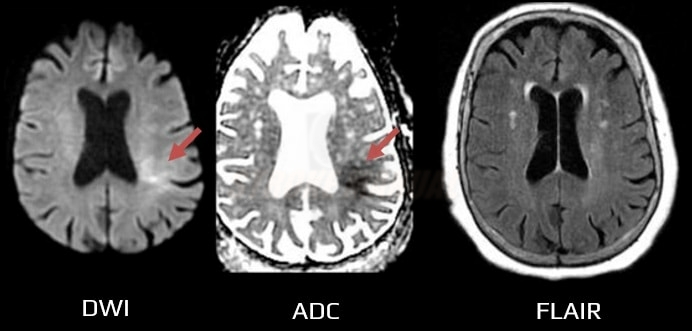
- a positive DWI with negative findings on FLAIR indicates that the stroke probably occurred within the previous 4.5 hours [Aoki, 2010] [Thomalla, 2009]
- may be useful to guide intravenous thrombolysis (IVT) in patients with stroke of unknown onset or wake-up stroke (WUS)
-
- DWI/FLAIR mismatch is present (DWI positive in <1/3 of the MCA territory, FLAIR negative)
- n=503 ( 254 tPA vs. 249 placebo), median NIHSS 6
- good outcome 53.3 vs. 41.8 (placebo), median mRS/3m 1 vs. 2
- mortality 4.1% vs. 1.2% (placebo)
- sICH 2% vs. 0.4% (placebo)
- MR WITNESS
- unwitnessed onset
- DWI/FLAIR mismatch (DWI positive in <1/3 of the MCA territory, FLAIR either negative or showing only minimal lesion)
- n = 80, sICH 1.25% (as defined by ECASS III)
- time window:
- 4.5 – 9 hours after the onset of stroke
- on awakening with stroke (if within 9 hours from the midpoint of sleep)
- ≥ 18 years, premorbid mRS < 2, NIHSS 4-26
- median NIHSS was 12 (tPA) and 10 (placebo)
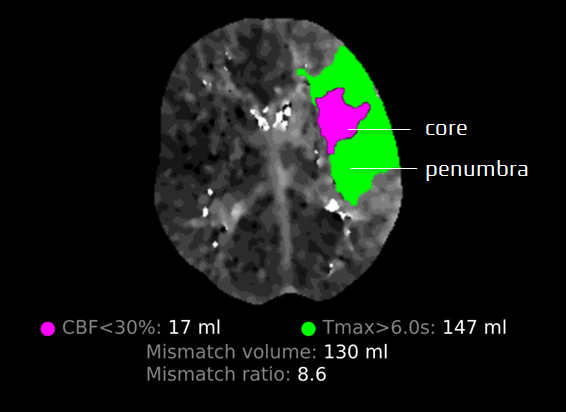
- CTP system RAPID or MR DWI/PWI mismatch → inclusion criteria
- mismatch > 1.2, absolute difference > 10 ml (Tmax > 6 s on perfusion)
- core < 70 ml (CT-CBF) – rCBF<30% on CTP or ADC<620mm2/s (DWI
- n=113 (tPA) vs. 112 (placebo) at 4.5-9h
- primary outcome (mRS 0-1 /3m): 35.4% vs 29.5%, RR 44%

- NNT 17 – efficacy similar to IVT at 3-4.5h
- sICH 6% (tPA) vs 1% (placebo)
- mortality 12% (tPA) vs. 9% (placebo)
Criteria for recanalization
Imaging
- IVT can be performed in WUS patients who meet the following imaging criteria (derived from guidelines):
- DWI/FLAIR mismatch – DWI lesion < 1/3 of MCA territory + negative FLAIR – meets WAKE-UP trial criteria (AHA/ASA 2019 IIa/B-R) (ESO guidelines 2021)
- FLAIR is usually negative in the first 2-3 hours (Levy, 1983)
- evidence of penumbra on CT perfusion (EXTEND trial criteria) (ESO guidelines 2021)
- the trial used a 9-hour time window, which fits most WUS patients (especially if we use the midpoint of sleep rule)
- DWI/FLAIR mismatch – DWI lesion < 1/3 of MCA territory + negative FLAIR – meets WAKE-UP trial criteria (AHA/ASA 2019 IIa/B-R) (ESO guidelines 2021)
- some authors advocate thrombolysis in WUS based on normal NCCT alone; the ESO 2021 guidelines do not recommend IVT in the 4.5-9 hour window or in WUS without penumbral imaging
- it appears safe to thrombolyse patients with wake-up stroke and a normal NCCT (Armon, 2019)
- the non-randomized TRUST-CT trial showed benefit in patients with ASPECTS ≥ 7 (OR 1.94 )
- RCTs are needed
Estimated midpoint of sleep
- the estimated midpoint can guide treatment decisions
- to calculate it, determine the interval between:
- the last time the patient was normal (bedtime or last interaction with others or, for example, visiting the toilet without difficulty) AND
- the time the symptoms were noticed upon awakening
- midpoint = divide this interval by two and add it to the last time normal
- examples
- last time seen 10:00 PM, symptoms noticed 6:00 AM, the estimated midpoint is 2:00 AM; if the patient arrives at the hospital at 7:00 AM, the estimated window is 5 hours ⇒ advanced imaging is required
- last time seen 11:00 PM, symptoms noticed 5:00 AM, the estimated midpoint is 2:00 AM; if the patient arrives at the hospital at 6:00 AM, the estimated window is 4 hours ⇒ NCCT is sufficient to indicate IVT
Management
Intravenous thrombolysis
- patients can be thrombolyzed if:
- brain NCCT shows no advanced early ischemia + interval from the midpoint of sleep to initiation of IVT is ≤ 4.5 hours
- advanced imaging criteria mentioned above are met + interval from the midpoint of sleep to initiation of IVT is < 9 hours
Mechanical recanalization
- thrombectomy is effective for medium- and large vessel occlusions (MeVo and LVO) and can be performed:
- within 7 hours 18 minutes based on NCCT alone (using the estimated midpoint of sleep)
- within 24 hours after the midpoint in patients selected by advanced penumbral imaging (DAWN, DEFUSE3 trials) → Mechanical recanalization
Patients not eligible for recanalization
- standard secondary prevention with antiplatelets or anticoagulation, depending on stroke etiology + management of vascular risk factors