GENERAL NEUROLOGY
Post-discharge care for patients recovering from subarachnoid hemorrhage
Updated on 23/10/2024, published on 22/10/2024
Surviving an SAH is a significant milestone, but recovery doesn’t end with discharge from the hospital. Survivors may experience a range of physical (hemiparesis), cognitive (deficit in memory, attention), and emotional challenges (depression, anxiety, personality changes) that require ongoing care and support. Proper post-discharge care is crucial for optimal recovery and prevention of complications.
Post-discharge care focuses on:
- preventing complications (monitoring for rebleeding, hydrocephalus, and seizures)
- rehabilitation and cognitive training to restore physical function, cognitive skills, and emotional well-being
- medication management – medications to control blood pressure, depression, anxiety, and to prevent seizures, etc.
- lifestyle modifications to reduce the risk of future hemorrhages
- regular appointments with neurologist, neurosurgeon, and primary care physician
- regularly evaluate neurological status to monitor the patient’s recovery
- screen for post-SAH cognitive dysfunction, depression, and anxiety and recommend psychotherapy or pharmacotherapy if needed
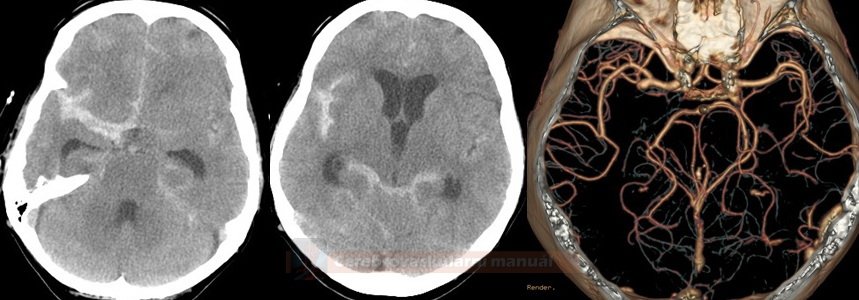
- imaging studies – CT/MRI to detect any complications such as delayed hydrocephalus
- postprocedural aneurysm imaging is discussed in a separate chapter
- usually, a contrast-enhanced MRA 3-6 months post-procedure to assess coil stability and aneurysm status is scheduled
- blood pressure monitoring
- keep BP < 120-130/80 mmHg to prevent rebleeding
- patients should measure their blood pressure regularly at home
- monitoring for complications
- rebleeding – sudden onset of severe headache, loss of consciousness, or neurologic deficits
- delayed hydrocephalus – nausea, vomiting, gait and balance problems, confusion, or urinary incontinence
- seizures – new onset or recurrent
- hyponatremia
- antihypertensives
- many SAH patients are prescribed antihypertensive medications to maintain blood pressure within safe limits
- adherence is essential to reduce the risk of recurrent bleeding
- antiepileptics
- if seizures occurred during the initial hospitalization, antiseizure medications might be prescribed, and compliance is critical → Stroke-related epilepsy
- pain management: Use approved medications for headaches and discomfort
- headaches are common after SAH
- patients should use prescribed medications and avoid over-the-counter pain relievers without consulting their healthcare provider, as some may increase bleeding risk
- nimodipine, used to prevent vasospasms, is usually discontinued at the time of discharge (or is soon to be discontinued)
- antiplatelet therapy after stent-assisted coiling (usually ASA+CLP for 3 months)
- compliance – the patient is advised to take medications as directed and to report side effects
- physical therapy helps improve strength, mobility, balance, and coordination
- occupational therapy focuses on helping patients perform daily activities such as bathing, dressing, and cooking; occupational therapy promotes independence and quality of life
- speech therapy addresses communication and swallowing difficulties
- cognitive rehabilitation helps enhance memory, attention, and executive function (problem-solving skills)
- anxiety and depression are common after SAH
- seek therapy for depression, anxiety, or mood changes (medication, psychological counseling)
- join a group for SAH survivors to share experiences and coping strategies
- encourage family members to provide emotional support and assist with caregiving
- smoking cessation
- smoking significantly increases the risk of recurrent SAH
- cessation support services should be recommended if necessary
- a healthy diet
- low-sodium, rich in fruits, vegetables, and whole grains
- obstipation prevention
- regular exercise in approved physical activities to improve cardiovascular health (walking or swimming)
- reduce or eliminate alcohol consumption

- support compliance – assist with medication management, accompany patients to follow-up visits
- provide emotional support – offer encouragement and understanding
- assist with daily activities
- monitor changes in the patient’s condition (improvements, signs of complications, etc.)