GENERAL NEUROLOGY
Decompressive craniectomy
Updated on 10/09/2024, published on 27/07/2024
Introduction
- decompressive craniectomy is a life-saving neurosurgical intervention used to reduce intracranial pressure in patients with malignant stroke or other causes of elevated ICP
- removing a portion of the skull allows the brain to swell outward, preventing further brain herniation with progressive neurological damage or death
Indications
- preferred in younger patients; consider very carefully in older patients
- do not wait for the effect of hyperosmolar therapy with developing malignant ischemia (as it has only minimal effect)
- the greatest benefit of hemicraniectomy is seen when it is performed within 48 hours of symptom onset
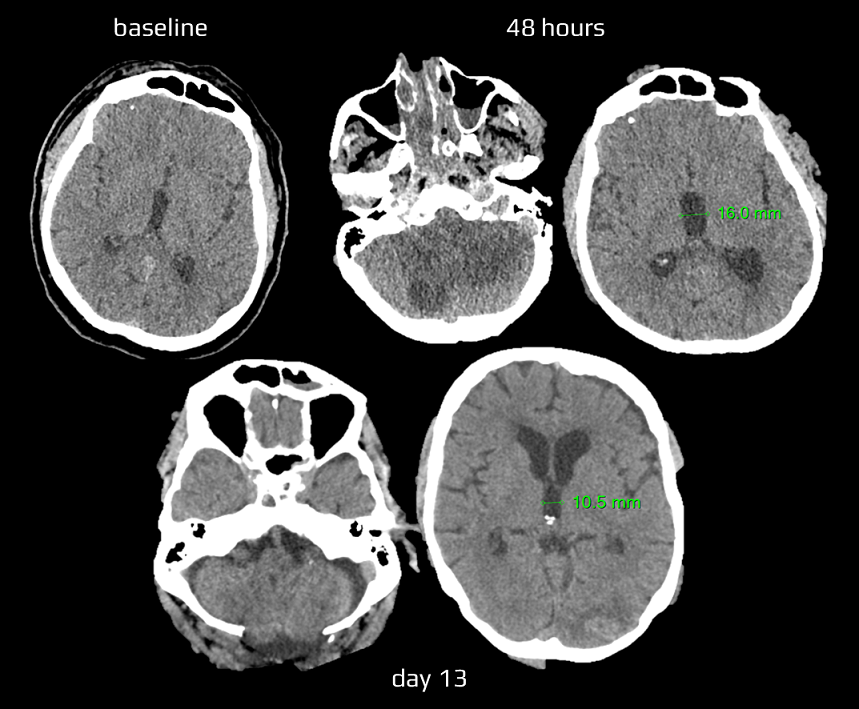
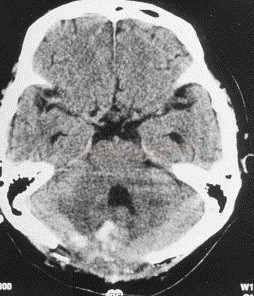
Cerebellar infarction
- alert and clinically stable patients are usually treated conservatively and monitored closely (although some authors recommend early or even preventive intervention)
- surgery is required in the case of extensive mass effect on imaging + clinical signs of brain stem compression (e.g., bradycardia, progressive loss of consciousness, etc.)
- imaging criteria of a mass effect
- compression of the 4th ventricle
- obstructive hydrocephalus
- basal cisterns/brainstem compression
- upward herniation of the superior vermis cerebelli through the tentorial notch
- downward herniation of the cerebellar tonsils through the foramen magnum
- procedures:
- suboccipital decompressive craniectomy +/- resection of necrotic tissue for expansive cerebral ischemia may be a life-saving procedure (AHA/ASA 2019 I/B-NR)
- ischemia leads to brainstem and aqueduct compression, so craniectomy can also relieve obstructive hydrocephalus
- it can be combined with the ventricular drainage
- ventriculostomy for obstructive hydrocephalus due to expansive cerebellar infarction (with or without craniectomy) (AHA/ASA 2019 I/C-LD)
- suboccipital decompressive craniectomy +/- resection of necrotic tissue for expansive cerebral ischemia may be a life-saving procedure (AHA/ASA 2019 I/B-NR)
- contraindications:
- clinical or radiological signs of severe, irreversible brain stem ischemia
- severe comorbidity or significant prestroke handicap
- known or presumed refusal of this intervention by the patient
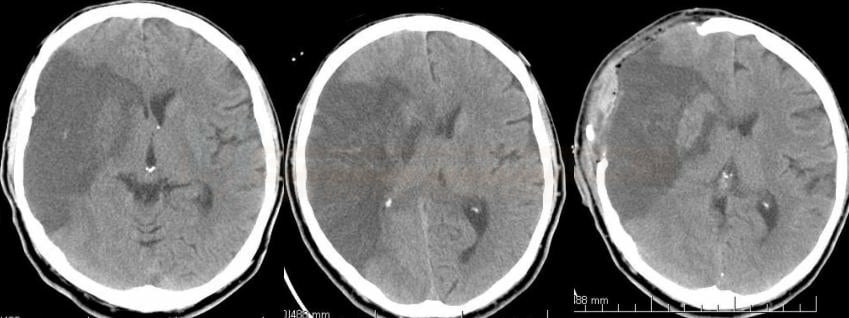
Supratentorial stroke (usually MCA territory)
- decompressive hemicraniectomy relieves pressure from the edematous tissue on adjacent tissue ⇒ ↓ ICP and ↑ CPP
- potentially life-saving procedure (see below for additional indication criteria)
- age < 60 years – a meta-analysis of the DESTINY, HAMLET, and DECIMAL trials demonstrated that decompressive craniectomy within 48 hours in patients aged <60 years resulted in reduced mortality and improved outcome (AHA/ASA 2019 IIa/A)
- age > 60 years – reduced mortality alone has been demonstrated in smaller studies [Won Yu, 2012] and randomized DESTINY II trial
- n = 112 (surgery 49 vs. control 63), age> 61 years
- mRS 0-4 39% (surgery) vs. 17% (control), ARR 22, NNT = 5 !!
- significant reduction of mortality (50%); compared to trials with patients < 60 years, there is a significant increase of survivors with very severe deficits and only a minimum of patients with mRS 3 (none 0-2) ⇒ questionable cost-effectiveness
- there are no indications that surgery should not be considered in patients with dominant-hemisphere infarction
- craniectomy diameter of at least 12 cm
- 14-15 cm anteroposteriorly
- 0-12 cm from the base to the vertex
- simultaneous resection of infarcted tissue is usually not recommended
Indication criteria for decompressive craniectomy (based on RCTs)
- age 18 – 60 years (younger patients have a better prognosis; at age > 60 years, mainly a reduction in mortality can be expected)
- NIHSS > 15
- progressive impairment of consciousness (somnolence-sopor)
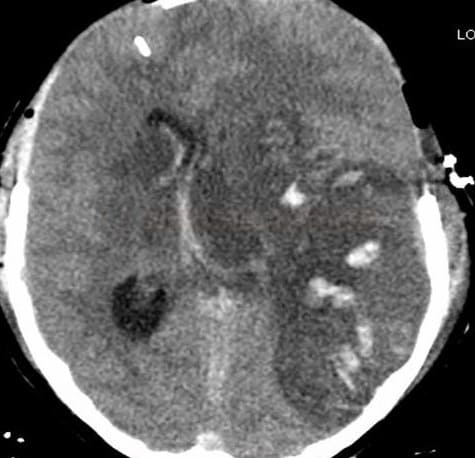
- ischemia > ½ of the MCA territory according to CT (with or without concurrent ipsilateral infarct in ACA or PCA territory)
- infarct volume > 145 cm3 on DWI
- mass effect (edema exceeding 50% of the MCA territory and midline shift)
- < 45 h (surgery completed in < 48 h) from symptom onset
Exclusion criteria (based on RCTs)
- bilateral non-reactive, not drug-induced pupillary dilation
- pre-morbid mRS ≥ 2 (3)
- extensive hemorrhagic component (type PH2)
- expected survival <3 years due to severe comorbidities (neoplasia, terminal heart failure, etc. )
- coagulopathy
- contraindications to general anesthesia (GA)
- refusal by the patient
- decompressive craniectomy, with/without hematoma evacuation, is typically reserved for patients with acute severe CVT and parenchymal lesions with impending herniation
- it is considered a life-saving procedure that increases the chance of a favorable outcome even in the most severe CVT cases
- DECOMPRESS2 trial showed that 2/3 of patients with severe CVT survived, and more than one-third were independent 1 year after decompressive surgery
- better results can be expected in:
- non-comatose young patients with unilateral lesions
- surgery within 48 hours of admission
- factors associated with poor outcome:
- age >50 years
- midline shift >10 mm
- total effacement of basal cisterns
- there is insufficient data to determine the preferred method between hemicraniectomy and endovascular treatment, as well as how and when to combine them
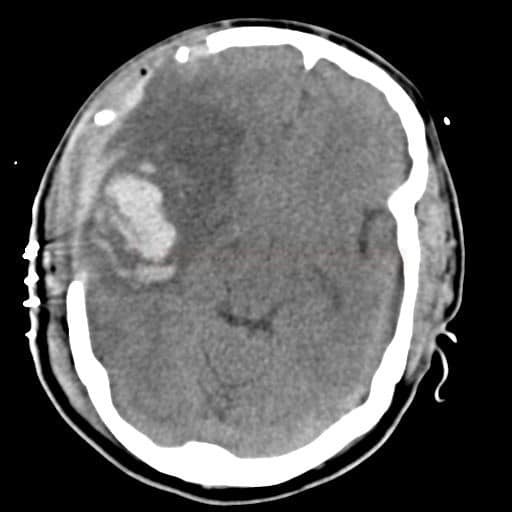
- not only hematoma volume but also subsequent edema formation contributes to mass effect and intracranial hypertension in ICH
- perihematomal edema usually peaks on the 3rd or 4th day, but has a very inhomogeneous time course and may persist for up to 2 weeks
- decompressive craniectomy (with or without hematoma evacuation) can be a lifesaving procedure in comatose patients with prominent mass effect (with midline shift) and drug-refractory IC hypertension
- decompressive craniectomy can be beneficial in reducing mortality in patients with large intracerebral hemorrhage or extensive ischemia associated with SAH, especially in cases with significant midline shift (Tuzgen, 2012)
- however, the effect on long-term functional outcomes remains less clear, highlighting the need for careful patient selection and timely intervention
- young age is an independent predictor of favorable outcome after craniectomy in SAH (Veldeman, 2022)
- decompressive craniectomy is an essential intervention in the management of severe TBI with elevated ICP
- the procedure significantly reduces mortality and increases the rate of severe disability; however, rate of moderate disability and good recovery seem to be similar in the surgical and medical therapy groups (
Procedure
- outcomes improve with timely intervention
- coagulation disorders should be corrected before craniectomy, if necessary, in collaboration with a hematologist
- a craniectomy after thrombolysis is possible and generally safe after IVT, without significant bleeding risks, even when performed early (Sadeghi-Hokmabadi, 2023)
- at the time of craniectomy, the coagulation factors should be in the normal range, particularly the fibrinogen
- if the patient received an antiplatelet drug, a preoperative platelet transfusion should be considered
- general anesthesia (GA) is administered, and the patient is positioned to allow optimal access to the surgical site
- a scalp incision is made, followed by removal of a bone flap to expose the dura mater
- the size and location of the craniectomy depend on the underlying condition and the area of brain swelling
- finally, the dura is loosely closed; the scalp is then sutured, and the bone flap is stored for future reimplantation
- fronto-parieto-temporo-occipital craniectomy up to the midline with a diameter of at least 12 cm is performed and a durotomy and an enlargement duroplasty are performed
- better ICP control is achieved in patients with a large decompressive craniectomy (Sedney, 2014) (Schur, 2014)
- aimed minimum size of the hemicraniectomy is 12 × 15 cm (Früh, 2023)
- removing ischemic brain tissue is not recommended
- in case of concomitant intracranial bleeding, the hematoma can be evacuated
- intracranial pressure monitor placement is recommended
- craniectomy up to the transverse sinus and opening of the foramen magnum is realized. In addition, durotomy, enlargement duroplasty, and removal of ischemic cerebellar tissue should be performed
- in case of concomitant hydrocephalus, external ventricular drainage with ICP monitor placement or a ventriculostomy should be considered
- shunt placement without realizing a craniectomy is not recommended
Postoperative management
- apply general intensive care concepts, inc. ICP and CPP monitoring, treatment of intracranial hypertension, and maintenance of an adequate CPP
- control CT is performed after 24 hours or earlier if signs of intracranial hypertension are present and before any attempt at waking from sedation
- thromboembolic prophylaxis with subcutaneous LMWH can be started on the 2nd postoperative day after consulting the neurosurgeon
- early rehabilitation should be initiated already in the ICU
- monitor and manage potential complications
Complications
- infection
- hydrocephalus – further intervention may be required, such as ventriculoperitoneal shunt placement
- subdural hygroma – the accumulation of cerebrospinal fluid in the subdural space is a common postoperative complication
- sinking skin flap (SSF) syndrome – also known as “syndrome of the trephined”
- it consists of a sunken skin over the bone defect with neurological symptoms such as severe headache, mental changes, focal deficits, or seizures
- may progress to “paradoxical” herniation as a result of atmospheric pressure exceeding intracranial pressure (Sarov, 2010)
- seizures – the risk of seizures increases postoperatively due to cortical irritation
- worsening of the neurological deficits
Cranioplasty timing and criteria
- the bone flap is typically re-implanted once brain swelling has subsided and the patient is neurologically stable (usually weeks to months post-surgery)
- the absence of infection, satisfactory neurological status, and adequate skin and soft tissue conditions are necessary before proceeding with cranioplasty
Prognosis
- the effectiveness of decompressive craniectomy varies depending on the underlying condition and patient characteristics (age, preoperative neurological status, etc.)
- in cases of malignant MCA infarction, the procedure reduces mortality in all age groups and disability in younger patients
- in TBI and ICH, outcomes are less predictable, with some studies indicating reduced mortality but uncertain effects on long-term functional outcomes